Detox is more than a physical process; it resets both the body and mind, laying the groundwork for a successful recovery journey.
From medical monitoring to therapeutic support, we’re here to help individuals move through detox safely and build a strong foundation for long-term recovery.
Quitting drugs or alcohol on your own might seem like a test of willpower, but it can be dangerous. It can trigger serious health risks, including seizures, dehydration, heart complications, and intense psychological distress.
That’s where detox therapies come in. These medically supervised programs provide a structured, supportive environment where individuals can withdraw safely, with access to medical care and emotional support.
Deciding to stop using substances is a courageous first step, but going it alone can be dangerous, even life-threatening. Detox therapies provide the medical and emotional support needed to navigate withdrawal safely, yet many people attempt to quit on their own, unaware of the serious risks involved.
Here are some risks of un-supervised detox:
Deciding to begin detox is a big step, and it shouldn’t be taken alone. A professional detox program provides the structure, support, and medical expertise necessary to make the process safer and more manageable.
Detox therapies go beyond clearing substances from the body. They set the foundation for long-term healing:
When it comes to overcoming substance use, detox is often the first—and most crucial—step. But detox isn’t just about “toughing it out.” Without the right support, withdrawal can be physically and emotionally overwhelming, even dangerous.
That’s where medical detox therapies provide expert care to help patients safely transition into recovery.
In a medically supervised detox, patients receive round-the-clock monitoring from healthcare professionals who are trained to manage withdrawal symptoms and prevent complications.
This structured environment ensures that individuals detox safely while receiving the comprehensive care from experts they need.
These medications are particularly effective for opioid, alcohol, and benzodiazepine detox, making it easier for individuals to transition into long-term treatment.
With the right approach, MAT doesn’t just manage withdrawal; it sets the stage for lasting recovery.
By choosing a medically supported detox, individuals give themselves the best chance at a healthier, more stable future. Detox therapies provide the medical expertise and compassionate care needed to begin the recovery journey safely and successfully.
A holistic approach to detox recognizes that the mind and body are deeply connected, and supporting both is essential for a sustainable recovery.
Here’s how key holistic therapies can play a role in the detox process:
Healing from substance use means replenishing what the body has lost. Nutritional therapy focuses on restoring essential vitamins and minerals that may have been depleted, helping to repair organ function and improve overall energy levels.
Hydration is equally important—substance use often leads to dehydration, which can make withdrawal symptoms feel even more intense. Proper nutrition and hydration support physical recovery and strengthen the body’s healing ability.
Detox can be emotionally overwhelming, too. Practices like yoga, meditation, and breathwork offer powerful tools for managing stress, easing anxiety, and stabilizing emotions.
These techniques help regulate the nervous system, making it easier to navigate cravings and discomfort during detox. Mindfulness-based practices also improve focus and resilience, creating a stronger foundation for long-term recovery.
By incorporating holistic detox therapies into the healing process, individuals can experience a more balanced and supportive recovery that nurtures body and mind.
When it comes to detox therapies, addressing the physical aspects of withdrawal is just one piece of the puzzle. Healing also requires emotional and behavioral support because addiction also takes root in the mind.
That’s why therapeutic interventions play a critical role in helping individuals get through detox and also build a foundation for lifelong wellness and sobriety.
For many, substance use is closely tied to past trauma. Trauma-informed therapy acknowledges this connection and provides a safe, supportive space for individuals to process painful experiences.
Instead of focusing solely on stopping substance use, this approach helps people understand why they turned to substances in the first place, empowering them to heal in a way that feels safe and sustainable.
Emotional and behavioral therapies are as essential as medical interventions in detox therapies. By addressing the underlying thoughts, trauma, and isolation that often accompany addiction, these approaches set the stage for a healthier, more resilient future.
If you’ve ever tried to cut back on caffeine and found yourself with a pounding headache, you’ve experienced a small taste of withdrawal. Now, imagine that discomfort amplified—both physically and emotionally—when withdrawing from substances like alcohol, opioids, or benzodiazepines.
Because withdrawal symptoms can be intense and sometimes dangerous, professional detox therapies are essential in helping individuals navigate this difficult process safely.
Below are some of the most common physical symptoms during detox:
Psychological symptoms can be just as prevalent as physical symptoms:
Know that, with professional support, these symptoms can be managed and reduced.
Detox isn’t a one-size-fits-all process. Every person’s journey with substance use is different: what led them there, how their body responds, and what they need to heal. That’s why personalized detox plans matter.
When detox therapies are tailored to a person’s unique needs, the process becomes safer, more effective, and more manageable.
A well-designed detox plan includes:
When it comes to overcoming substance dependence, choosing the right detox approach is a crucial first step. Detox therapies are designed to manage withdrawal symptoms safely, but not all detox programs are the same.
The decision between inpatient and outpatient detox depends on factors like the severity of withdrawal, personal responsibilities, and risk of relapse.
For individuals facing severe withdrawal symptoms or a high risk of relapse, inpatient detox offers 24/7 medical supervision and emotional support.
This structured setting removes outside triggers, providing a safe, controlled environment where individuals can fully focus on recovery without the distractions or stressors of daily life.
Medical professionals monitor progress, manage symptoms, and adjust treatment plans as needed to ensure safety and comfort.
Outpatient detox allows individuals to continue their daily responsibilities—work, school, or family—while receiving medical care and therapeutic support. This works best for those with mild to moderate withdrawal symptoms who have a stable home environment and a strong support system.
Regular check-ins with medical providers and counseling sessions help keep individuals on track and address any challenges that arise during the detox process.
Recovery doesn’t end when the body is clear of substances; in many ways, the real work is just beginning. Without ongoing care, the risk of relapse remains high, making it essential to have a solid plan in place for what comes next.
After detox, a person’s next steps depend on their unique needs, but some key components of a successful recovery plan include:
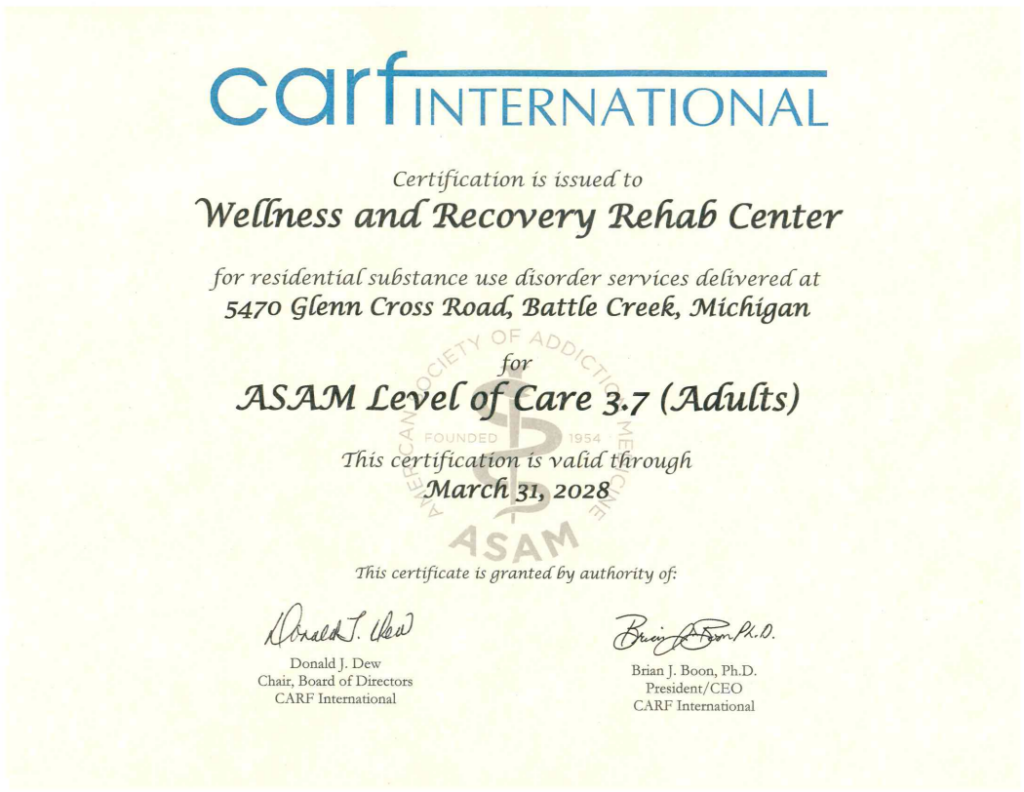
Taking the first step toward recovery is often the hardest thing to do, but it’s also the most important. At Wellness and Recovery, we understand that detox is more than just a physical process—it’s the foundation for lasting change.
That’s why we offer compassionate, evidence-based detox therapies tailored to help you safely and comfortably begin your journey toward a healthier, addiction-free life.