Chronic pain isn’t just ongoing discomfort – it’s a complex condition that impacts your body and mind. Unlike acute pain, which serves as a temporary signal of injury or illness and diminishes with healing, chronic pain lingers for months or even years, often without a clear resolution.
This connection is not incidental; the neural pathways that process pain also regulate emotions, creating a cycle in which persistent pain heightens stress, irritability, and emotional exhaustion.
The interplay between pain and mental health extends beyond momentary discomfort. Prolonged activation of the brain’s stress response can cause changes in mood, cognition, and resilience. Over time, the body’s heightened sensitivity to pain can reinforce feelings of frustration and helplessness.
Common symptoms of chronic pain can range from physical to emotional, including:
Too often, individuals struggling with chronic pain turn to substance misuse as an unhealthy coping mechanism—only leading to a dangerous cycle that can be hard to break without the right support.
The complexity of chronic pain underscores the importance of a thorough and accurate diagnosis. Identifying the causes of chronic pain requires a comprehensive assessment that goes beyond surface-level symptoms.
Physicians may utilize imaging scans, laboratory tests, and detailed medical histories to determine whether pain originates from musculoskeletal conditions, nerve disorders, inflammatory diseases, or psychosomatic factors.
Below are some of the most prevalent causes of chronic pain:
Arthritis is a leading cause of chronic pain, affecting millions of people worldwide. Osteoarthritis occurs when joint cartilage wears down, leading to stiffness, inflammation, and reduced mobility.
Rheumatoid arthritis is an autoimmune disorder in which the immune system attacks joint tissues, resulting in chronic pain and swelling.
Fibromyalgia is a neurological disorder characterized by widespread musculoskeletal pain, extreme fatigue, and cognitive dysfunction. The cause is not fully understood, but researchers believe it is linked to an overactive nervous system that amplifies pain signals.
Conditions such as herniated discs, spinal stenosis, and degenerative disc disease are common causes of chronic pain. Poor posture and sedentary lifestyles can worsen symptoms over time.
Neuropathy occurs when nerves become damaged due to diabetes, chemotherapy, infections, or trauma. This results in burning pain, tingling, numbness, and muscle weakness, particularly in the hands and feet.
MS is a chronic autoimmune disease where the immune system attacks the central nervous system, leading to nerve inflammation, muscle spasms, and chronic pain.
Migraines are recurring, severe headaches that can last for hours or days, often triggered by stress, poor sleep, and hormonal changes.
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, causing chronic pelvic pain, painful periods, and inflammation.
While the causes of chronic pain often stem from medical conditions or neurological disorders, lifestyle and environmental factors also play a crucial role in pain severity and overall well-being.
The causes of chronic pain are not always limited to physical injury – daily habits, stress levels, and external influences can either exacerbate or alleviate symptoms. Many individuals unknowingly engage in behaviors that intensify discomfort or overlook stressors that contribute to prolonged suffering.
A truly effective pain management plan goes beyond addressing the underlying medical condition; it also involves modifying daily routines and reducing external triggers.
Some of the most common causes of chronic pain from environment or lifestyle include:
Physical inactivity is one of the leading causes of chronic pain. The body is designed for movement, and when it remains sedentary for long periods, muscles weaken, joints stiffen, and circulation decreases, all of which can worsen pain.
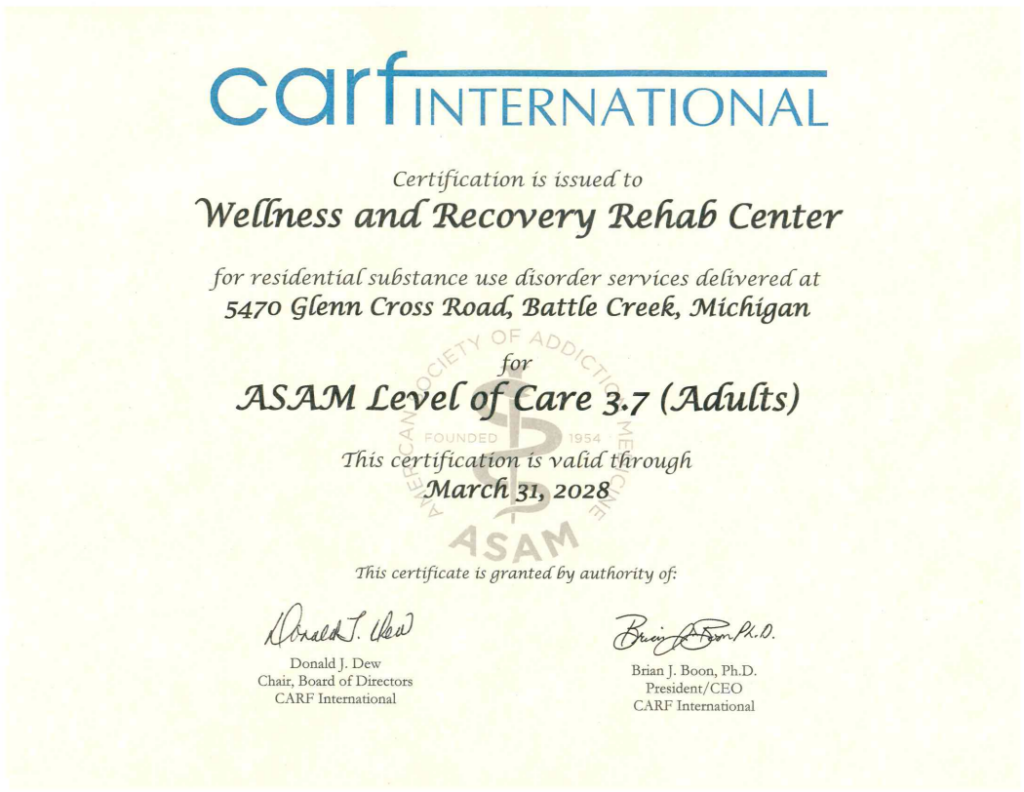
At Wellness and Recovery, we encourage gentle movement therapy, stretching exercises, and pain-friendly fitness programs as part of a comprehensive treatment approach. Low-impact activities like yoga and aquatic therapy can help improve flexibility, reduce inflammation, and enhance pain tolerance.
Excess body weight places additional stress on joints, muscles, and nerves, particularly in individuals with arthritis, back pain, or knee conditions. Obesity is also linked to chronic inflammation, a major factor in conditions such as fibromyalgia and autoimmune diseases.
Nutritional factors that influence chronic pain include:
Chronic pain and sleep disorders are closely connected. Many individuals suffering from pain report difficulty falling asleep, staying asleep, or reaching restorative sleep, which in turn heightens pain sensitivity, fatigue, and emotional distress.
Sleep deficiency affects many aspects of pain and healing, including:
At Wellness and Recovery, we help individuals implement simple yet effective lifestyle changes to help ease their co-occurring pain. Strategies include reducing screen time before bed, maintaining a consistent sleep schedule, and establishing a calming nighttime routine.
Many individuals struggling with chronic pain turn to opioids, alcohol, or other substances to numb their discomfort. While pain medications can provide temporary relief, long-term reliance on opioids can lead to dependence, tolerance, and addiction.
Substance use can worsen chronic pain symptoms through:
Chronic pain does not exist in isolation – mental health, stress levels, and external factors heavily influence it. This phenomenon is due to the nervous system’s prolonged hyperactivation, increasing muscle tension and pain sensitivity.
The mind-body connection can significantly impact chronic pain, including:
For many individuals living through the causes of chronic pain, the pursuit of relief often leads to long-term reliance on prescription pain medications, including opioids.
While these medications can offer temporary symptom management, they also come with significant risks, such as dependence, addiction, and even heightened pain sensitivity over time.
The complex relationship between the causes of chronic pain and substance use has become a growing health concern, emphasizing the need for integrated treatment approaches that prioritize physical and psychological well-being.
These numbers underscore the urgent need for safer, non-addictive alternatives to pain management.
As the medical community works to address the opioid epidemic, there is increasing emphasis on non-opioid treatment options that effectively manage chronic pain while reducing the risk of addiction.
Some of the most promising approaches include:
Medications such as buprenorphine, methadone, and naltrexone help stabilize brain chemistry while reducing opioid cravings and preventing relapse.
Non-opioid pain medications can be used to relieve discomfort and include:
Physical therapy is one of the most effective long-term solutions for chronic pain relief. This therapy helps improve strength, mobility, and flexibility, reducing the need for pain medications.
Pain rehabilitation programs also incorporate massage therapy, hydrotherapy, and exercise therapy to help patients regain functionality.
At Wellness and Recovery, we provide dual diagnosis treatment, meaning we treat co-occurring chronic pain and mental health conditions simultaneously.
By treating the physical and psychological aspects of chronic pain, individuals have a greater chance of achieving long-term relief and recovery.
Our comprehensive pain and recovery program includes:
We address the causes of chronic pain through evidence-based treatments that enhance physical function, emotional resilience, and overall quality of life. Through personalized care, we empower individuals to take control of their pain in a way that supports sustainable healing and lasting relief.
Overcoming chronic pain and addiction is not just about treatment – it is about ongoing support and lifestyle changes that help individuals maintain long-term wellness.
We offer a full continuum of care, including:
By staying engaged in long-term care, individuals are more likely to experience lasting relief from chronic pain and sustained recovery from substance dependence.
Chronic pain and addiction are closely intertwined, often reinforcing each other in a cycle that can be challenging to break without comprehensive support.
Addressing the causes of chronic pain through an integrative approach is essential, offering sustainable solutions that prioritize physical healing and emotional well-being without the risks associated with prolonged substance use.
At Wellness and Recovery, we are committed to helping individuals reclaim their lives through comprehensive, compassionate, and research-backed treatment.